Medical Education
Methodist University’s plans to open a medical school in partnership with Cape Fear Valley Health may have raised an eyebrow or two among educational and medical professionals.
Both Fayetteville-based institutions are small relative to their peers, and starting a medical school from scratch is an ambitious project.
But proponents say this tall order appears to be the right order, given the urgent shortage of doctors, nurses and other health care providers. The problem is particularly acute in the rural counties of southeastern North Carolina, all of which are federally designated Health Professional Shortage Areas.
“There’s a great need in all (medical) specialties, in all areas, so someone starting a new school that will produce more doctors — hey, that’s good news,” says Dr. Alison Whelan, chief academic officer for the Association of American Medical Colleges, a Washington D.C., nonprofit that represents 640 institutions.
“The basic idea of this school, as I understand it, is to bring more providers to a particular area that’s in need, to a rural area, and there is research that indicates that’s a strategy that does work. So, this is a smart strategy, a useful strategy.”
Methodist and Cape Fear have their work cut out for them. Methodist’s plans an initial class of 80 students in 2026 with goal of about 120 per class as the school develops. The school could be home to nearly 500 students when enrollment is maxed out. Medical schools remain oversubscribed, says Whelan, so filling slots shouldn’t be a problem.
That’s good news. But paying for the school will not be as easy. It’s expensive to hire instructors and establish labs and other space.
Moreover, the existing doctor shortage that plagues so many communities will undoubtedly trouble the medical school as it looks for residency slots for its new graduates down the road.
Third- and fourth-year medical students rotate through a series of “clinical clerkships” that form the bulk of their education during those last two years of school. After that, doctors must serve residencies lasting three to seven years before they’re full-fledged physicians.
The training requires doctors or other seasoned medical professionals to serve as preceptors who teach and direct the students.
Methodist’s basic thesis is that students trained in Fayetteville will be more likely to begin their practice in Cumberland County and neighboring counties served by Cape Fear and its six other hospitals or rehab centers. Cape Fear had revenue of $1.17 billion in the 2020 fiscal year. Plans call for adding nearly 100 beds at the main 524-bed Fayetteville hospital in the next few years.
Alternatively, med school grads may head off for a residency in a far-flung post with a bigger name and not return.
“That will be a challenge,” says Whelan. “You’d like to keep them all there, and that is the best plan. But there is a serious shortage with regard to the availability of residencies and preceptors. Not every doctor wants to do this. When you spend time with students, guess what? You don’t see as many patients.”
Having Cape Fear Valley as a partner will be helpful, she adds. “Everyone — doctors, the school, the hospitals involved — needs to understand this and see the long-term picture. It’s good that they have a hospital as a partner. I can’t imagine doing it any other way.”
The Fayetteville system has offered clinical rotations and post-grad residences for many years. That means that some slots are already spoken for. For instance, Cape Fear has more than 200 residents from Campbell University’s Jerry M. Wallace School of Osteopathic Medicine. Osteopathic schools supply slightly different training than medical schools, but put students on the path to becoming a doctor.
Suzanne Blum Malley, Methodist’s provost, calls Cape Fear’s residence program, “a huge advantage as we start a medical school based in Fayetteville.” Prospective residents are “matched” with available residencies through a nationwide system. Methodist’s goal is for its medical students to “match” in the Cape Fear system, but Malley says the school realizes that won’t happen in every case.
Two-thirds of students who complete their medical degrees and residencies in the same area stay in that area to practice, according to the medical school trade group.
Methodist officials also expect that the influx of residents and medical students will improve access to medical care. That’s one of many “halo benefits” that Methodist and Cape Fear officials project for the hospital’s service area. Including construction,
the medical school could lead to more than 800 new jobs. A study by an N.C. State University economist projected the school would add $750 million to the regional economy in the school’s first 10 years.
“The advent of the school will have a transformative effect on the community over time, improving the quality of medical care, attracting and retaining medical care providers and new areas of specialization, attracting other medically-related businesses, increasing the median income level, adding to the tax base, and bringing in new revenue from the purchase of goods and services,” says Stanley Wearden, Methodist’s president since 2019.
It should also boost enrollment at the university’s health care specialties. Methodist has about 2,300 students and offers an undergraduate degree in nursing and advanced
degrees for nurse practitioners, physician assistants, occupational therapists,
and physical therapists.
Funding the expansion is expected to involve a mix of federal grants, tuition income and private donations.
Faculty and support personnel have to be hired. Preceptors rarely work for free either, and residents are paid a stipend. Cape Fear’s current residency program pays $54,000 to $66,000 annually, not including a standard full-time benefits package.
Methodist, which has an endowment of about $35 million, will own and operate the
medical school. The Cape Fear system is contributing to start-up expenses, including the school’s main building, which is expected to cost $50 million. The not-for-profit system
had about $614 million of net assets on its balance sheet as of mid-2020. its latest public tax filing shows.
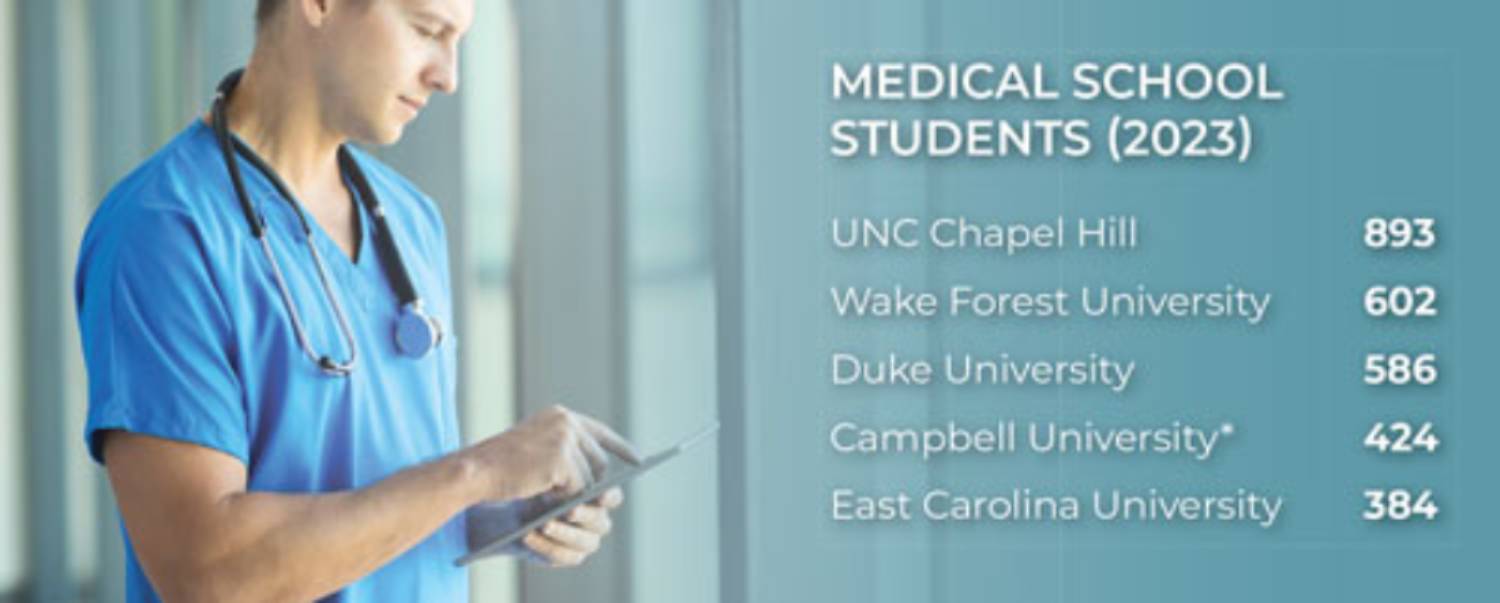
In Charlotte, the heavily promoted plan for a Wake Forest University medical school campus is backed by Advocate Health, which has capital exceeding $12 billion, and major corporate support in the state’s biggest city.
Malley says Methodist can handle the Cumberland County project. “Through our partnership (with Cape Fear Valley Health) we are prepared for those expenses,” Malley says. “We are also exploring all sources of potential external funding, including government and philanthropic sources.”




